Radiofrequency Ablation
Patient information on obliteration of thyroid nodules and cysts (radiofrequency ablation)
One in three people in Austria has nodules and/or cysts in the thyroid. Most of these are benign. If, however, they grow quickly or cause discomfort, including difficulty swallowing, shortness of breath, globus sensation (“lump in the throat”) or the nodules visibly protrude from the neck (cosmetic problem), in many cases the only option until now was to operate on the thyroid.
Around 10,000 thyroid operations are currently performed per year in Austria. They are performed under general anaesthesia during an in-patient stay lasting several days. Sick leave of approximately 2 weeks is customary in Austria. Besides general complications as in all surgical procedures (haemorrhages, disorders of wound healing, dermal scarring, etc.), serious complications with a high degree of psychological strain for patients can occur during thyroid operations (hoarseness due to damage to the vocal cord nerve, calcium deficiency and associated tingling or cramps due to removal of the parathyroids). In most cases, lifelong replacement therapy with thyroid hormones is necessary following a thyroid operation.
Through the use of radio frequency waves, a minimally invasive technique for treating thyroid nodules and cysts has been available for a few years. Radiofrequency ablation of the thyroid was performed for the first time in 2002 by Professor Baek in South Korea and has since been continuously developed. Roughly 7000 surgical procedures are performed per year worldwide in just a few centres; this method has been available in Austria since 2014.
The exact treatment procedure is as follows:
You do not need an empty stomach for the surgical procedure – a light breakfast is allowed. Thyroid tablets or other medication (particularly for diabetes or high blood pressure) should also be taken.
Warning! Blood-thinning medication may not be taken on the day of examination and may need to be paused for a few days before the procedure.
Your circulation parameters (blood pressure, pulse, oxygen saturation, etc.) will be monitored for the duration of the procedure. General anaesthesia or sedation (slight somnolence as is feasible in gastrointestinal endoscopies) is not required. You will be able to breathe, swallow and even talk normally for the duration of the radiofrequency ablation procedure. Dr Lehner will ask you several times during the procedure how you are doing, whether you feel pain, and will check your voice while doing so.
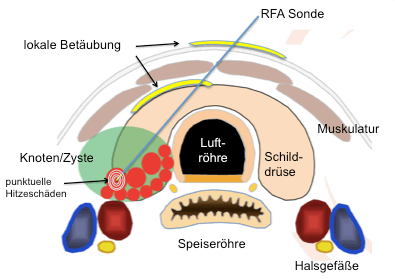
Following local anaesthetic under the skin and under ultrasound guidance to the thyroid capsule (yellow curved lines on the diagram below), a probe is inserted, with guidance by ultrasound, into the nodule to be treated, which has the roughly the thickness of a ballpoint pen refill. Heat is generated at the probe tip and the nodule is treated step by step, as shown in the diagram, by means of a high frequency wave created in a generator. This technique is also called the ‘moving shot technique’.
In general, approximately 2–3% of patients experience discomfort during the obliteration procedure. The thyroid itself is not sensitive to pain, though the surrounding capsule and the skin under anaesthesia are. This is associated with temporary burning (similar to that experienced during anaesthetisation by the dentist). In the event of severe discomfort, the procedure will be interrupted and anaesthetic injected again until the patient is completely free of pain. The procedure does NOT cause any scarring to the neck.
Figure left: llustration of a cross-section of the neck and thyroid region. The trachea (tunnel-shaped structure), the oesophagus (flat “toothed” muscle tube behind it and the horseshoe-shaped thyroid around the trachea are illustrated. The yellow lines show the location of the two anaesthetic deposits. The needle generates small pads of heat at its tip, making it possible to treat the nodule (green oval) step by step.
Who is a good candidate for radiofrequency ablation?
For safety reasons, radiofrequency ablation is not performed during pregnancy. It does not present problem for breastfeeding. An implanted pacemaker or defibrillator rules out treatment with high frequency waves. Please let us know if you are taking blood thinning medication during the initial consultation; in this case, it must be paused for a certain period depending on the product.
Radiofrequency ablation is not an absolute alternative to thyroid surgery. If a surgical procedure has been recommended to you, a decision will be made by the treating physician on whether radiofrequency ablation is feasible as an alternative on the basis of the present findings. Further examination may be necessary in the thyroid practice. The nodules to be treated must also be punctured twice with the guidance of ultrasonography in order to rule out malignancy with a high degree of probability. This is not required for smaller “hot” nodules (autonomous adenomas) as these nodules are predominantly benign.
What effect does heat exposure have on the nodules?
Thyroid tissue is permanently destroyed at temperatures in excess of 64°C. The protein is “denatured”, which is similar to when you boil an egg. Special defence cells of the body subsequently break down the dead nodule tissue, which leads to the shrinking of the nodules. The extent of reduction depends on the original size and nature of the nodule; around 40–60% after 3 months and around 60–90% after 1 year. Residual connective tissue is the only remnant of the former nodule. The surrounding healthy tissue remains completely unharmed and can continue to produce hormones so that daily intake of tablets is not required following the procedure.
With the reduction of the nodule volume, any existing difficulty swallowing, feeling of pressure, feeling of tightness of the throat or nodule visible to the naked eye usually significantly decrease or, at best, are no longer detectable.
How long does the procedure last?
The actual radiofrequency ablation lasts between 30 and 60 minutes depending on the size of the nodule. You ought to set aside around 3 hours on the day of treatment. Following the procedure, a chilled cryo-bag is placed on the treated area of the neck with light pressure. We would be like to monitor you for at least 30 minutes following the procedure. You will then receive decongestant and anti-inflammatory medication. Please do not drive yourself home after the procedure.
Please avoid the following for three days following the procedure:
- Lifting heavy objects (over 5 kg)
- Strenuous physical and general sporting activities (including cycling!)
- Manoeuvres that involve holding one’s breath (“clenching”), e.g. playing a wind instrument, inflating something, etc.
- Overstressing your voice (no singing, shouting, etc.)
- Do not take a full body bath on the evening of the date of the procedure. However, showering (with a waterproof plaster) is possible
What disorders or complications can occur?
– Temporary voice changes (hoarseness)
– Slight bleeding (which usually disappears on its own in the course of 1 day to 3 months at the latest)
– Wound infections
– Rare: Vomiting, cough, seared skin at the needle puncture site
Although very rare, an inpatient stay or follow-up treatment may become necessary due to a complication during or after the procedure.
Given the proximity to and cooperation with the Klinikum Wels-Grieskirchen, an intensive care team and an experienced thyroid surgeon are immediately available in the event of unexpected serious complications or cardiovascular incidents.
A one-off treatment is completely sufficient for a satisfactory decrease in the nodule volume for most average sized nodules. In the case of particular proximity of some nodules to vocal cord nerves or in the case of very large nodule formations, a second or – in the latter case – repeated procedures may be necessary. However, this can almost always be assessed by your physician beforehand and would then be addressed by him/her.
What follow-up examinations are required?
Following radiofrequency ablation, patients should undergo ultrasound examinations at the suggested intervals after 3 and 12 months. This also serves to document the reduction of the nodule. The ultrasound examination should always be performed by your own physician.
How much does radiofrequency ablation cost and how is it reimbursed by health insurance schemes?
The total costs amount to € 2700 and must be paid on the day of examination in cash or by debit card. Unfortunately, the procedure is associated with very high material costs (probe, generator, sterile procedural and draping materials, etc.). The ablation probes cost approximately €1,300 and can only be used once, meaning that only one probe can be used per patient (however, several nodules can be treated).
At present, only a few statutory health insurance schemes reimburse this procedure. We will gladly assist you with the application for reimbursement, but no guarantees can be made, however. Most supplemental insurance policies reimburse a significant portion of the costs. Please consult your health insurance scheme or supplemental insurance policy provider in this regard before the procedure.